RESEARCH-ARTICLE
Hyun Guy Kang1∗ and San Ha Kang2
Show details
Abstract
Bone is one of the most common metastatic areas in the cancer patient. Bone metastasis is the major cause to deteriorate the quality of life due to severe pain, walking difficulty, paraplegia, and pathologic fracture. To maintain patient’s general condition and continue scheduled medical treatment, various minimally invasive surgical methods have been developed. The percutaneous methods including alcohol or bone cement (polymethyl methacrylate [PMMA]) injection, laser or radiofrequency ablation, cryosurgery, and MRI-HIFU have shown favorable outcomes in the spine, pelvis, and other flat bones. Using only these percutaneous methods have high risk of pathologic fracture in the long bone of extremity, which needs some metallic fixation. Therefore, the new surgical method and instrument involving percutaneous internal fixation with PMMA bone cement injection have been introduced. The PMMA bone cement injection is effective in the metastatic bone tumor, providing reliable mechanical augmentation of destructive bone, durable local tumor suppression, and effective pain relief. The hollow-perforated screw and nail (multihole injection screw and nail) has central canal and multiple side holes to facilitate injection of bone cement to the bone lesion. An optimal customized surgical option according to the patient’s circumstances should be planned.
Keywords: metastatic bone tumor, minimal invasive surgery, hollow-perforated screw, percutaneous fixation and injection, palliative management
1. Introduction
Metastatic bone cancer is the most common malignancy in the bone tumor. The life expectancy of patients has been increasing considerably over the recent years since the development of cancer management, but the occurrence chance of bone metastasis also increased. The incidence rate ranges from 20% to 85%, varying by type of cancers. Bone metastasis is the major cause to deteriorate the life quality of patients due to severe pain, walking difficulty, and pathologic fracture. Pathologic fracture is induced in around 10% of bone metastasis, and is life-threatening to patients.
The treatment of metastatic bone tumor includes the combination of modality including medication, radiation therapy, and surgery to reduce pain and prevent bone destruction. Recently, the use of bisphosphonate and denosumab was reported as an inhibition of osteolytic microenvironment factors. Radiation therapy is the most frequently used and effective method for palliation but has limitation of bone strengthening.
Generally, patients need operation for the prevention of pathologic fracture, especially on the weight-bearing bones like vertebrae, pelvis, and femur as well as long tubular bone of extremity. The early surgical management before the fracture is important and has many benefits: avoiding terrible pain and complications, relatively easy surgery, reducing rehabilitation time and life-threatening condition. The surgical methods for bony metastasis include curettage and bone cement (PMMA, polymethyl methacrylate) augmentation, internal fixation with plate or intramedullary (IM) nail, arthroplasty, and prosthesis reconstruction. The surgical treatment method is chosen by multidisciplinary teamwork. The most appropriate surgical option should be selected under the consideration of patient’s age and life expectancy, general condition, response of medical treatment, and even preoperative life quality, because major surgery lead to stop or delay of chemotherapy and radiation therapy, and many accompanied complications.
Recently, various minimally invasive surgical methods that can be performed without general anesthesia and large incision have been introduced for metastatic bone tumor: ethanol injection, cryoablation, radiofrequency (RF) ablation, cementoplasty, etc. The percutaneous bone cement (PMMA, polymethyl methacrylate) injection is known as cementoplasty or osteoplasty, and has been shown favorable outcomes in the vertebral body and the flat bones such as pelvis, scapula, and sternum. However, solitary bone cement injection without metallic fixation at the long bone still has high risk of pathologic fracture.
A new novel surgical technique will be introduced in the concept of percutaneous metallic fixation and simultaneous bone cement injection. For this technique, the unique implant, multihole injection screw and nail, is developed. This implant has a hollow in the center and perforated side holes allowing the material injection to the bony lesion. This minimally invasive surgical method showed good result in the respect of pain relief, mechanical stability, surgical risk, rehabilitation period, hospital stay, surgical cost, and local tumor suppression. The injection material can be various, including chemotherapeutic agent, anti-osteolytic agent, and accelerate bone healing agent as well as PMMA bone cement. Recently, the MR-guided focused ultrasound surgery (MRgFUS) is introduced. MRgFUS is an external ablation which showed effectiveness in reducing pain from bone metastases. However, MRgFUS lacks restoration for mechanical stability.
This chapter will introduce the diverse developing minimally invasive surgical methods and suggest future direction for better management of patients with metastatic bone tumor.
2. Various methods of minimally invasive surgery for metastatic bone tumor
2.1. ALCOHOL ABLATION (ETHANOL INJECTION)
Alcohol ablation is a simple and inexpensive technique for tumor ablation. The ablation involves cellular dehydration and ischemia that lead to endothelial necrosis and vascular thrombosis. Before the injection of the alcohol, a mixture of iodinated contrast material (25%) and lidocaine 1% (75%) is introduced to examine area of the alcohol diffusion, and patient will be put under local anesthesia. Alcohol ablation has been a treatment for bone metastases rather than primary bone tumor. However, the method has a risk of failure or complications as the alcohol may uncontrollably diffuse into the tumor and surrounding soft tissues [1].
2.2. LASER ABLATION
Laser ablation is the application of thermal energy converted from light energy. Thermal energy will be diffused into the tumor tissue, inducing cellular coagulation necrosis through denaturation of cellular protein. For this technique, a neodymium: yttrium aluminum garnet (Nd:YAG) type generator or diode is used at lower power for thermal effect (photocoagulation) or at higher frequency (vaporization and cavitation).
The procedure time is short (about 10 minutes) and the extent of tumor necrosis is related to the amount of deposited energy, up to 15 mm in diameter for 1200 J. In the case of photocoagulation, laser ablation has been a useful method to treat benign primary bone tumor osteoid osteoma because of its accuracy, reliability, and accessibility. However, photocoagulation is not appropriate to treat large lesions [1].
The current use of laser ablation for metastatic bone cancer is limited; the laser technology cannot cover large lesion and takes long time to be done percutaneously.
2.3. RADIOFREQUENCY (RF) ABLATION
Radiofrequency ablation is a procedure to damage tumor cell through heat generated from an active electrode inserted into the tumor. For effective treatment, the procedure is performed at a temperature between 60°C and 100°C for 5–10 minutes.
Different size of a single tip electrode, which ranges from less than 15 mm up to 50 mm in diameter, determines the removable size of tumor. To treat larger volume of tumor, additional electrode should be inserted: internally cooled electrodes for cooling system and pulsed mode, perfused electrode, which increases tissue conductivity, or umbrella-shaped electrode and multipolar arrays which increases electrode tip coverage.
Radiofrequency ablation has been widely used to treat soft tissue cancer including hepatocellular carcinoma and thyroid cancer. In the skeleton, this method is used both as curative treatment for benign bone tumor such as osteoid osteoma, and palliative treatment for metastatic bone tumor [1]. Figure 1 illustrates an operation case for bone metastasis by RF ablation.
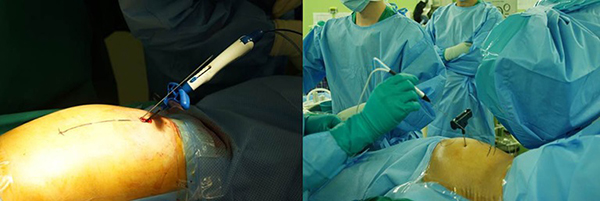
FIGURE 1.
RF ablation can be applied for the pelvic bone metastasis.
2.4. CRYOABLATION
Liquid nitrogen has been used as an intraoperative adjuvant method in the open bone tumor surgery. For the percutaneous application, technical progress was made for probe manufacturing, and utilization of argon gas as a cryogen. The argon gas freezes the tumor tissues at −100°C around the active probe, forming ice balls around the probe. Temperature below −20°C leads to cellular necrosis causing protein denaturation and rupture of cell membranes.
In general, the size of the necrosis is likely to be smaller than the ice ball and its maximum is up to 3 cm in diameter. The forming ice ball can be monitored by ultrasonography or computer tomogram but cannot be detected by fluoroscopy. Processes of the cryoablation are categorized into three phases: a first freezing phase (10 minutes), a thawing phase with helium gas (5 minutes), and a second freezing phase (10 minutes). Cryoablation is commonly used to treat prostate cancer. Treating metastatic bone tumor using cryoablation, however, may not be a good choice; the method fails to cover its big sizes, takes a long time, and is unable to perform moving tip technique [1]. Figure 2 illustrates a treatment for femoral neck metastasis by cryoablation.
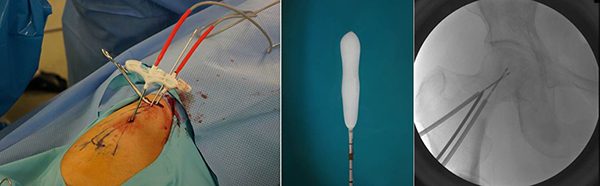
FIGURE 2.
Cryosurgery with probe type rod is applied for femoral neck metastasis.
2.5. MRI-HIFU (HIGH-INTENSITY FOCUSED ULTRASOUND) ABLATION
HIFU induces coagulation necrosis of the tumors by focusing high heat transformed from ultrasound produced by a transducer on tumors.
HIFU ablation has been a treatment for uterine myoma as well as palliation of bone metastases and sarcomas. The biggest advantage of HIFU ablation is its noninvasive procedure (however, the development of its interstitial applicators is in progress). In addition, HIFU ablation can eliminate tumors clearly and promptly: about 15 mm in diameter along the axis of the beam and about 1.5 mm in transverse diameter. Its procedure is conducted under MR or US guidance [1].
3. Polymethyl methacrylate (PMMA) bone cement injection
Percutaneous bone cement injection is known as a cementoplasty or an osteoplasty. The PMMA has been used in orthopedic surgery from 1945 including joint replacement surgery, spinal compression fractures, chronic osteomyelitis with antibiotics and tumors. The structure of methyl methacrylate monomer allows polymerization at room temperature to produce solid PMMA. The avidity of the polymer to dissolve in monomer aids this reaction. The composition of PMMA is shown in Figure 3 and Table 1.

FIGURE 3.
The PMMA bone cement is activated by mixing powder and liquid components.
Percutaneous vertebroplasty was originally developed as a treatment for angiomas, but its application to the osteoporotic spine has been shown to provide significant and prolonged relief of pain. It controls the symptoms of compression fractures by recreating mechanical stability. The technique involves the percutaneous transpedicular injection of low viscosity biomaterial into the vertebral body guided by an image intensifier.
Percutaneous bone cement injection for the metastatic bone tumor has been shown favorable outcomes in the vertebral body and the flat bones such as pelvis, scapula, and sternum. The PMMA has been one of the most useful agents in the treatment of bone tumors since it provides immediate mechanical stability and reduces bone pain. The reason for pain improvement after percutaneous cementoplasty (PC) procedure is due to tumor suppression, microfracture recovery, nerve ending sacrifice, mechanical strengthening, etc. When the heat is generated from solidification of bone cement, cytotoxic effect causes the destruction of tumor. The PMMA can also have a mass effect by interrupting circulation to the tumor. Nonetheless, the risk of pathologic fracture is still high when PC is solely performed in long tubular bones such as femur, tibia, and humerus without metal fixation [2].
| Composition | Function |
|---|---|
| Polymer | Polymethyl methacrylate |
| Copolymers (e.g., methacrylate-methyl methacrylate) | Alter physical properties of the cement |
| Barium sulfate or zirconium dioxide | Radio-opacifiers |
| Antibiotics | Antimicrobial prophylaxis |
| Dye (e.g., chlorophyll) | Distinguish cement from bone |
| Monomer | Methyl methacrylate monomer |
| N,N-dimethyl-p-toluidine (DMPT) | Initiates cold curing of polymer |
| Benzoyl peroxide | Reacts with DMPT to catalyze polymerization |
| Hydroquinone | Stabilizer preventing premature polymerization |
| Dye (e.g., chlorophyll) | Distinguish cement from bone |
TABLE 1.
Bone cement composition.
3.1. PERCUTANEOUS CEMENTOPLASTY FOR PELVIC BONE METASTASIS
The pelvic bone is a connecting area between spine and femur. The acetabulum of pelvis is a direct contact area with femoral head and important for weight bearing. When the metastatic tumor occurred at the acetabulum, the percutaneous PMMA injection will be a good option [3].
3.1.1. SURGICAL TECHNIQUE
The PC is performed under regional spinal anesthesia. A patient is positioned in lateral decubitus position. A sterile field is prepared and skin is punctured with 10 or 11 gauge osteoplasty needle at the 10 cm posterior from anterior superior iliac spine. The needle is advanced from posterior to anterior at an angle about 70° from the horizontal plane. The osteoplasty needle is usually used over two needles to reduce intraosseous pressure at the time of bone cement injection: the bone cement is injected through a single needle, until bloody fluids, and injected bone cement regurgitate through the other needles. Empty syringe will aspirate the unnecessary fluids and then bone cement is injected through all needles. Under fluoroscopic guidance, with anterior-posterior and oblique views of a pelvis, the PV needle penetrates the outer cortex and the tip is positioned in the lesion. The low-viscosity radiopaque PMMA is mixed and transferred to a 30 ml or 50 ml syringe, depending on the number of cement pack (20 g per a pack). Then, PMMA is transferred again into several 1 ml syringes. With the frequent check of oblique fluoroscopic view to avoid sciatic nerve injury by leakage, bone cement is injected as much as possible. If injection is not easily accomplished, a stylet is used to push PMMA through the lumen of needle. The bone cement injection is usually conducted within 3–4 minutes after making the cement mixture.
PMMA injection has to start slowly to prevent venous leakage with careful C-arm fluoroscopy monitoring. If the bone cement flows rapidly to the regional vein on the fluoroscopy, the injection has to be delayed to achieve thicker mixed bone cement. Figures 4 and 5 show the operative process of percutaneous cementoplasty.
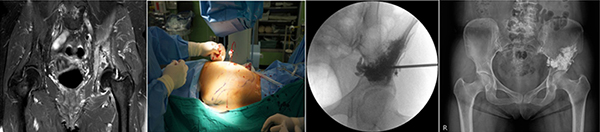
FIGURE 4.
A 54-year-old female has left pelvic bone metastasis of breast cancer. Bloody osteolytic lesion managed by PMMA bone cement injection.
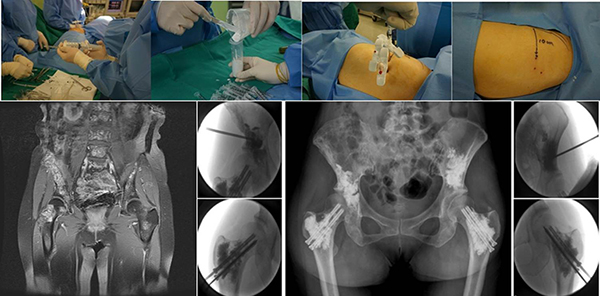
FIGURE 5.
Intraoperative photographs showing preparation of bone cement and start of injection through one needle for intraosseous pressure decompression. Multiple bone metastases are frequently involved around hip joint and these can be treated with one time surgery by minimally invasive surgery.
The anesthesiologist is asked to monitor temporary change of blood pressure, pulse rate, and respiration due to toxicity and volatility smell of PMMA. In the case of a larger lesion encroaching most of the ilium, another VP needle can be employed in the same way.
3.2. EVALUATION OF PERCUTANEOUS PMMA BONE CEMENT INJECTION
F-18-FDG PET-CT is known for good detectability of bone metastases in several types of cancers, and became widely used for treatment response evaluation and recurrence detection. The quantitative PET-CT values, SUVmax, and SUVmean showed significant uptake decrease after PMMA injection procedure, which means less glucose uptake and reflects tumor suppression. However, most control lesions were aggravated in the same individual patient.
Previous studies report that after bone cement injection, tumor volume is reduced and histology showed tumor necrosis, which support our hypothesis. Bone scan (BS) is known for good detectability, therapy response monitoring, and long-term follow-up of bone metastases. BS is advantageous for whole skeletal metastases detection [4]. BS and F-18-FDG PET-CT have complementary value as BS can detect osteoblastic metastasis well, and both are good imaging modality to detect bone metastasis.
Interpatient study was unable to be performed due to the differences in patient status (primary tumor, treatment, etc). So we performed comparison study of PS lesion and control lesion in the same patient. In our study, as shown in Figure 6, BS showed improved or stable state after PMMA injection procedure, which means local tumor suppression. However, most control lesions showed aggravated state [5].
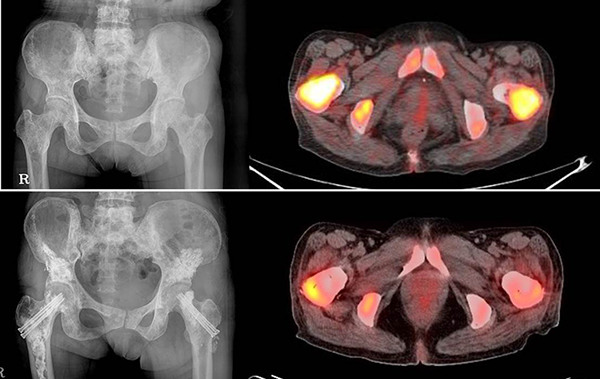
FIGURE 6.
PET-CT evaluation after combined percutaneous cement injection surgery showed effective tumor suppression in the metastatic bone tumor. Before (above) and after (below) operation.
4. Percutaneous internal fixation and PMMA bone cement injection for long bone metastasis
4.1. FEMORAL NECK METASTASIS
The femur neck is very vulnerable area to fractures due to senile osteoporosis and metastatic bone cancer [6]. The conservative treatment of metastatic tumors in the femoral neck is difficult because of the frequency of intractable pain and impending or established pathological fracture. Any of the aforementioned methods of treatment may be considered but do not significantly contribute to the stability of the femoral neck. Usually, the patients are treated by either joint replacement or internal fixation for pain palliation. The bipolar hip arthroplasty is a mainstay for femur neck metastasis but is too much a burden to the advanced terminal cancer patient. Recently, a new novel surgical technique for the treatment of femoral neck metastasis using hollow-perforated screws (HPSs) and bone cement was introduced [5–7].
4.1.1. HOLLOW-PERFORATED SCREW,/h3>
The hollow-perforated screw (HPS), as illustrated in Figure 7, is a newly developed device, modified from a 6.5-mm cannulated screw (Multihole Injection Screw; SOLCO, Seoul, Korea). The screw allows to achieve greater fixation capable of injecting material into the weak bone area simultaneously through its multiple side holes.

FIGURE 7.
The hollow-perforated screws have multiple holes for injection. The equipment facilitates percutaneous fixation and simultaneous bone cement injection for femur neck.
4.1.2. SURGICAL TECHNIQUE

FIGURE 8.
A 58-year-old female has impending fracture of right femoral neck metastasis by lung cancer. Percutaneous fixation and PMMA bone cement injection are effective methods for prevention of pathologic fracture.
The procedure is performed in the lateral decubitus position under spinal anesthesia. The femoral neck anteversion is drawn with the guidance of C-arm fluoroscopy. Two or three 2.2-mm guide pins are inserted to the femoral neck as the same pattern of cannulated screw fixation in the femoral neck fracture. The length of the inserted guide pin is measured and a small skin incision is made for cannulated drilling. After the cannulated drilling, two or three multihole injection screws are introduced over the guide pins. After checking the location of all screws fluoroscopically, the osteoplasty needles are inserted into the canal of screw. These osteoplasty needles are driven into the silicone tube before insertion, which is made temporarily by segmentally cutting a hemovac line for preventing leakage of injected materials at the connecting site with the screw. The guide pin is removed and low-viscosity PMMA bone cement is injected through 1 ml syringes. Figure 8 shows preoperative and postoperative photographs by percutaneous fixation and PMMA bone cement injection and Figure 9 shows detailed surgical procedures.
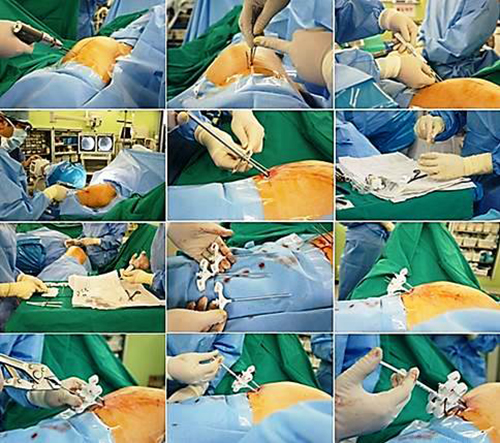
FIGURE 9.
Detailed surgical procedure demonstrated for femoral neck metastasis.
4.2. PERCUTANEOUS FLEXIBLE NAIL FIXATION AND BONE CEMENT INJECTION FOR HUMERUS
The rigid conventional intramedullary nailing method has been widely used for treatment of traumatic fracture as well as long bone metastasis. When surgeons place rigid nail to the humeral lesion, general anesthesia, locked screws, and sometimes curettage and cementing are required. The current study reported the palliative surgical treatment of metastatic humeral lesions using percutaneous Ender nailing along with bone cement augmentation under regional anesthesia in patients with high-risk advanced cancer [4].
4.2.1. SURGICAL TECHNIQUE
After interscalene or axillary regional anesthesia, the patient is placed in the supine position so that fluoroscopy cannot be disturbed. The entry points of the Ender nails (4.5-mm diameters; Smith & Nephew plc, London, UK) are the greater tubercle of the humeral head for proximal and diaphyseal lesions, and the lateral condyle for supracondylar lesions. Ender nails that are long enough to pass the intramedullary metastatic lesion are selected. When the Ender nail is completely seated, the tip at the entry point should be buried beneath the cortex to prevent soft tissue irritation. The osteoplasty needles are directly inserted into the medullary cavity by hand-push or hammering in a percutaneous and transcortical manner. Over two needles are commonly used for decompression of intramedullary pressure during bone cement injection and coverage of larger or skipped lesions. The entry point of the needle is selected at the most easily accessible area to the lesion, which is apart from the neurovascular bundles. After identifying the location of the needles by fluoroscopy, low viscous bone cement is injected through one needle and sequential through other needles.
4.3. PERCUTANEOUS FLEXIBLE NAIL FIXATION AND BONE CEMENT INJECTION FOR FEMUR AND TIBIA
The small diameter of intramedullary flexible nail fixation provides the space for percutaneous bone cement injection. The combinational percutaneous surgery with flexible nail insertion and bone cement injection can be useful to long bone metastasis patients who cannot undergo conventional intramedullary nailing due to poor life expectancy and multiple surgical demanding fracture risk areas. Although the pathologic fracture can be progressed more by weak stability of flexible nail than by rigid conventional nail, in the selective patient condition, this surgical method is effective to maintain bedside care and reduce further osteolytic progression. Patients with subtrochanteric lesion, pathologic fractures, or joint destructive lesions are excluded.
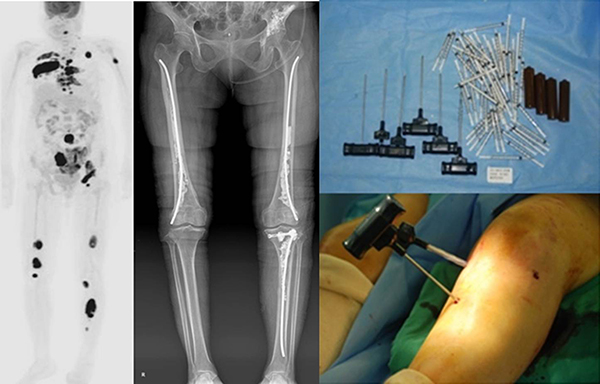
FIGURE 10.
The four areas (left pelvis, both femurs, and left tibia) can be treated at once.
The Ender nail fixation in the humerus, femur, and tibia has some limitation for the bone cement injection. Each osteoplasty needle has to penetrate skin and bone cortex for placing to the intramedullary perimetal area [8]. Figure 10 shows percutaneous flexible nail fixation and bone cement injection.
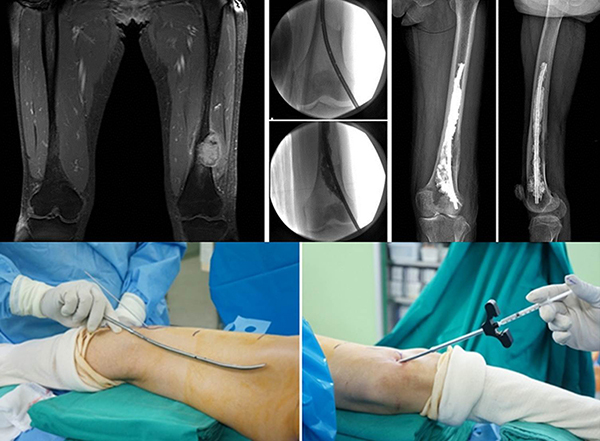
FIGURE 11.
The multihole injection nail was developed for simultaneous bone cement injection in the course of nail insertion without adding cortical punctures.
Very recently, the multihole injection nail (SOLCO, Seoul, Korea) has developed into a hollow titanium flexible nail with the tip of multiple side holes. The bone cement could be injected deeply in the course of a percutaneous fixation without adding bone cortex holes. The advantages of this new implant include immediate achievement of stable fixation and effective pain relief, deeper injection of drugs or bone cements, a short recovery time, and high emotional satisfaction from simple operation [9]. The use of the multihole injection nail is shown in Figure 11.
4.4. CLOSED INTRAMEDULLARY (IM) NAILING WITH PERCUTANEOUS CEMENT AUGMENTATION
The rigid IM nailing is widely used for metadiaphyseal lesions of the long bones and for trochanteric and subtrochanteric lesions of the femur in particular. Immediate bony stability and pain relief may be achieved with low morbidity. IM nailing may be undertaken using an open or closed technique. Closed IM nailing tends to be used when there are minimal bone destruction and displacement of the fragments. It may combine with percutaneous cement augmentation. Closed nailing with cement augmentation has many advantages over only closed nailing. First, intra- and post-operative bleeding is reduced as cement fills the space around the nail. Second, the cement gives early mechanical stability by preventing further destruction of bone and supporting the bone that remains; this results in further relief of pain. Third, filling the canal with cement at the time of nailing may limit the intramedullary spread of tumor [10]. Its operative procedures are shown in Figure 12.

FIGURE 12.
The combined percutaneous bone cement injection with the conventional intramedullary nailing leads more effective in the symptom relief and local tumor suppression.
5. Chemotherapeutic agent-loaded bone cement
Beyond the injection of bone cement only, there is growing interest on therapeutic effects on mixture of bone cement and chemotherapeutic agents. Many studies suggested that antineoplastic agent–loaded bone cement not only prevents tumor recurrences with better local tumor control but also decreases the number of distant metastases [11].
According to the literature, percutaneous injection with a mixture of gemcitabine and PMMA bone cement was applied to two patients of femoral neck metastasis from lung cancer [7]. In vitro test reported that the antineoplastic agents, such as cisplatin laden bone cement, hinder the growth of giant tumor cells, colon cancer cells, lung cancer cells, and breast cancer cells [11]. But further studies are needed to investigate efficacy of the chemotherapeutic agents incorporated into bone cement.
6. Bisphosphonate-added bone cement
Bisphosphonates (BPs) are antiresorptive drugs widely used to treat bone diseases such as osteoporosis, bone metastases, and hypercalcemia of malignancy, to prevent bone loss, and to increase bone density [12, 13]. Several studies demonstrate that BPs with bone cement have effects on increasing mechanical property and reducing bone resorption.
BPs in combination with bone cement play a key role in mechanisms of reducing a risk of bone resorption. BP-enriched bone cement can regulate important mediators involved in osteoclastogenesis, such as RANKL synthesis by osteoblast, and may modulate OPG, a decoy receptor of RANKL absorption, thus preventing RANK activation. In addition, two BPs alendronate and pamidronate mixed with calcium phosphate bone cement showed satisfactory results in mechanical properties. Both of them raise osteoblast proliferation and differentiation while restraining osteoclastogenesis and osteoclast function [14]. BP-combined cement can be a promising drug device as a local approach, preventing osteoporotic vertebral defect [13].
However, there is a paucity of clinical cases on clear efficacy of BP-laden bone cementoplasty and further studies are needed.
7. Conclusion
The metastatic bone cancer takes the highest frequency of more than 95% of malignant bone tumors and has adverse influences on quality of life in patient with advanced disease. Moreover, metastatic bone tumor usually reveals in multiple areas. An optimal customized surgical option according to patient’s circumstances should be planned, in order to achieve durable skeletal stability, effective pain relief, least surgical morbidity, less hospital stay, and local tumor suppression.

